EM@3AM: Murine Typhus
EMDocs
DECEMBER 1, 2024
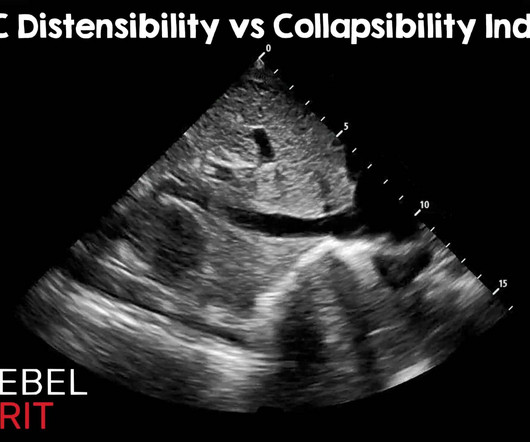
We’ll keep it short, while you keep that EM brain sharp. The RUSH exam: Rapid Ultrasound in SHock in the evaluation of the critically lll. The post EM@3AM: Murine Typhus appeared first on emDOCs.net - Emergency Medicine Education. Curr Opin Infect Dis. 2016 Oct;29(5):433-9. Perera P, Mailhot T, Riley D, Mandavia D. 2009.09.010.










































Let's personalize your content