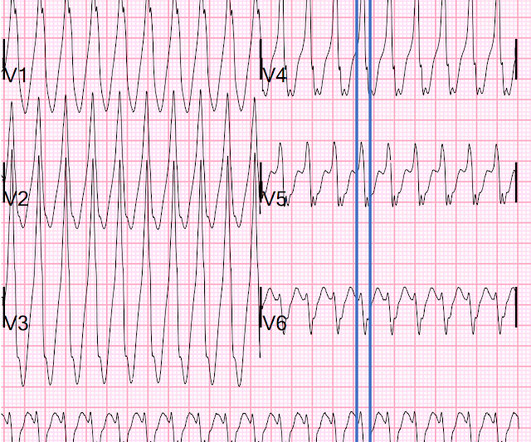
Torsade in a patient with left bundle branch block: is there a long QT? (And: Left Bundle Pacing).
Dr. Smith's ECG Blog
JANUARY 2, 2025
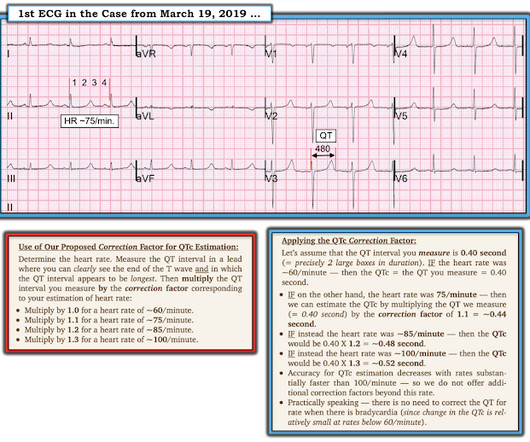
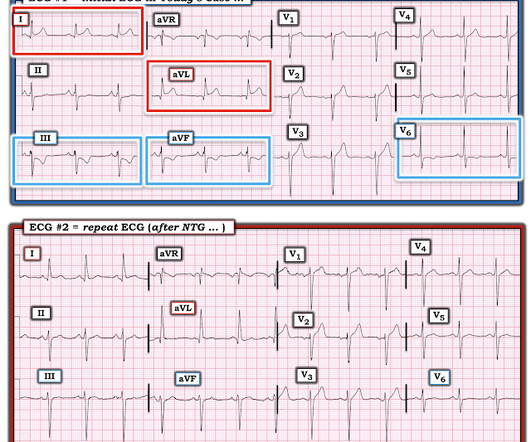
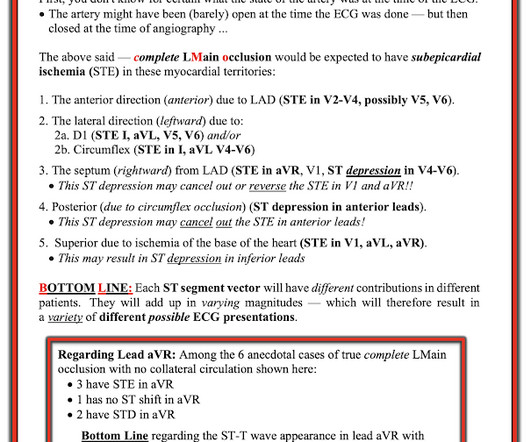
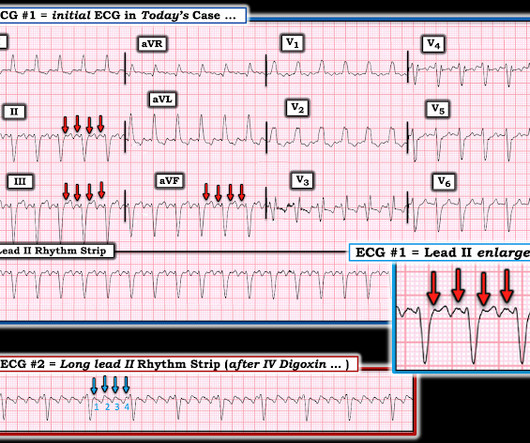
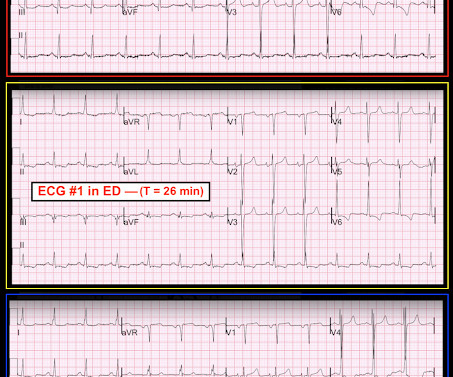
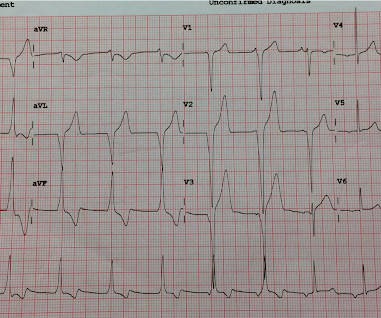
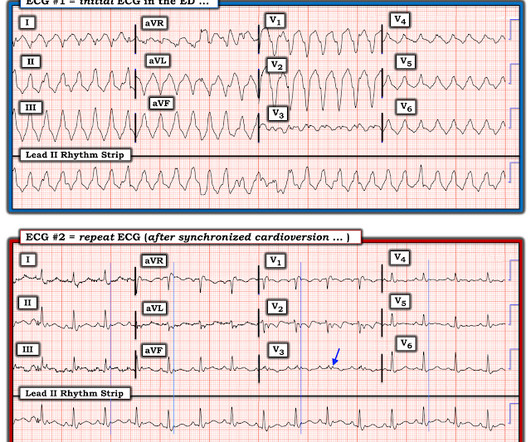
Bedside cardiac ultrasound showed moderately decreased LV function. She had an ECG recorded: This is left bundle branch block (LBBB), with appropriate proportional discordance. Here is one of the strips This is clearly polymorphic VT and probably torsade de pointes Subsequent ECGs. She was intubated. No wall motion abnormality.
















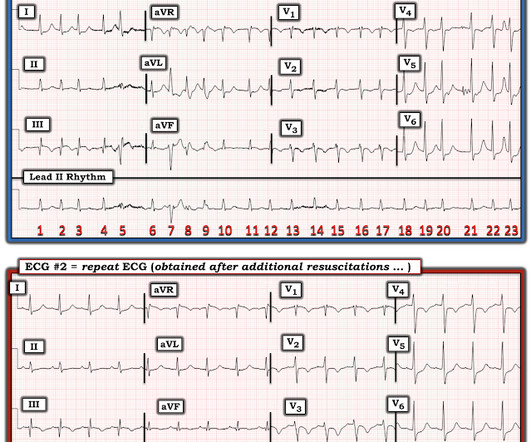






















Let's personalize your content