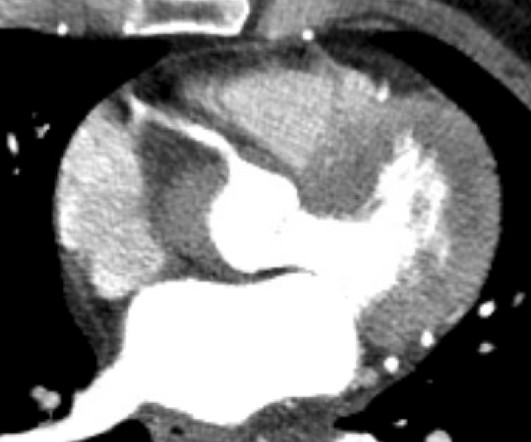
Concerning EKG with a Non-obstructive angiogram. What happened?
Dr. Smith's ECG Blog
DECEMBER 19, 2023
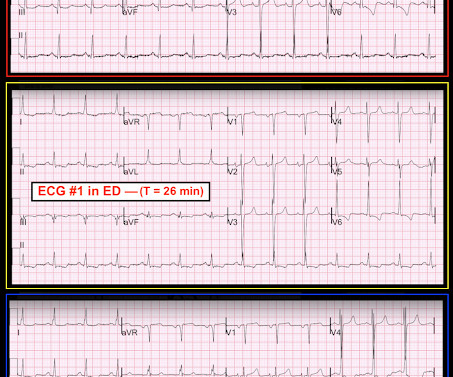
It appears EMS obtained two EKGs, but unfortunately these were not saved in the medical record. The EMS crew was only BLS certified, so EKG interpretation is not within their scope of practice. The patient arrived just after 10 AM, and the following EKG was obtained. There are no further EKGs or troponin measurements.





















Let's personalize your content