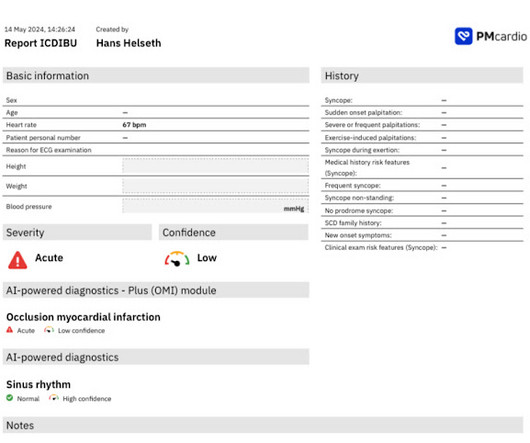
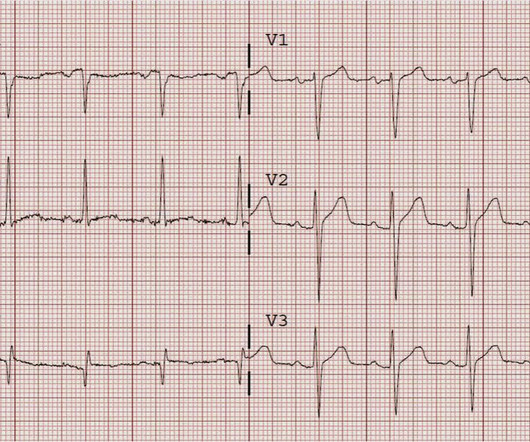
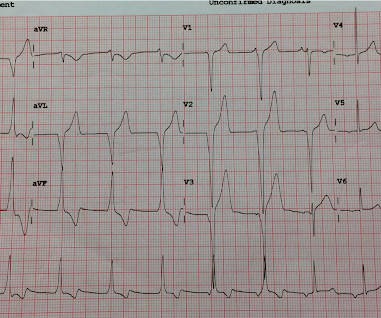
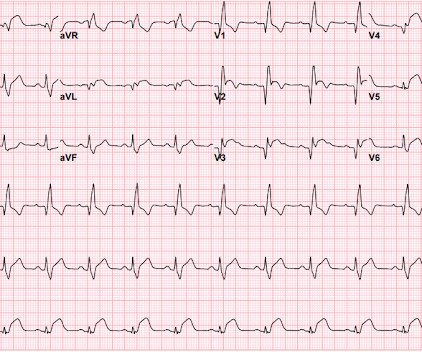
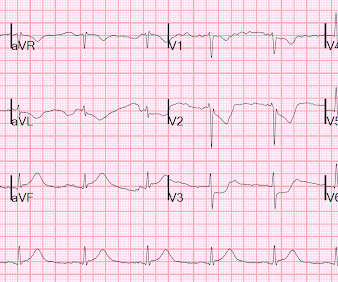
An undergraduate who is an EKG tech sees something. The computer calls it completely normal. How about the physicians?
Dr. Smith's ECG Blog
MAY 20, 2024
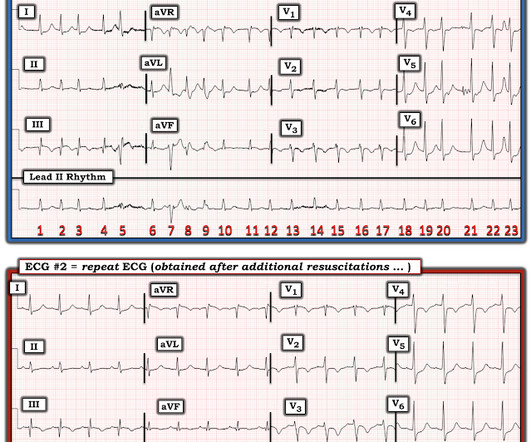
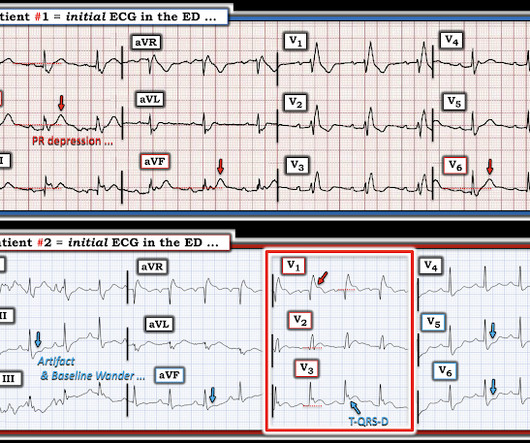
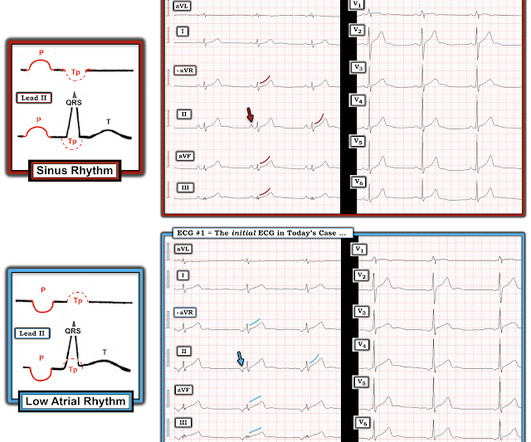
This was sent by an undergraduate (not yet in medical school, but applying now) who works as an ED technician (records all EKGs, helps with procedures, takes vital signs) and who reads this blog regularly. The undergraduate's analysis: This EKG shows J point elevation of about 0.5-1 Edited by Smith He also sent me this great case.





































Let's personalize your content