Putting Clinical Gestalt to Work in the Emergency Department
ACEP Now
OCTOBER 29, 2024
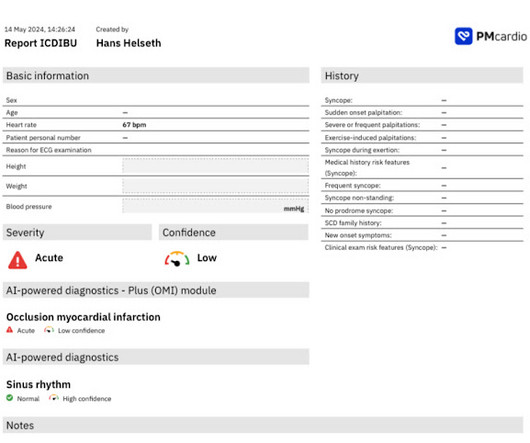
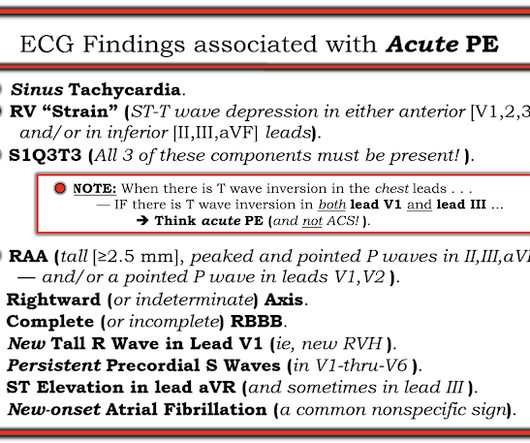
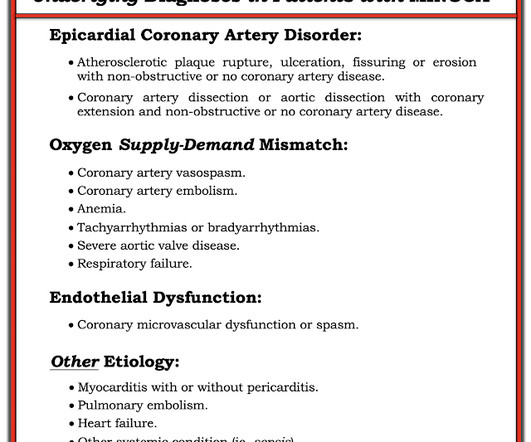
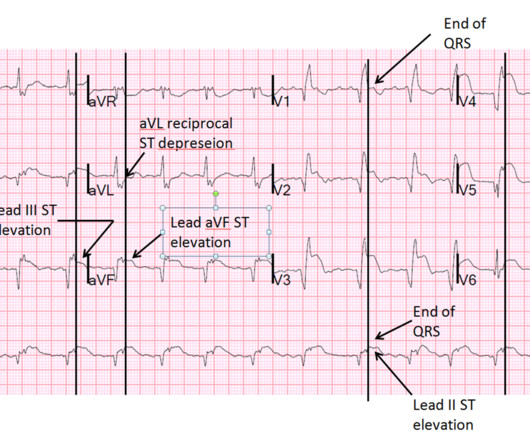
On a busy day shift in the emergency department, our seasoned triage nurse comes to me after I finish caring for a hallway patient, “Hey, can you come see this guy in the triage room? This is the essence of emergency medicine. The “bundling” heuristic—if I send a troponin, then an ECG is needed. His vitals are fine…”.









































Let's personalize your content