Variation Exists! Outcomes Exist!
EM Literature of Note
JANUARY 16, 2025
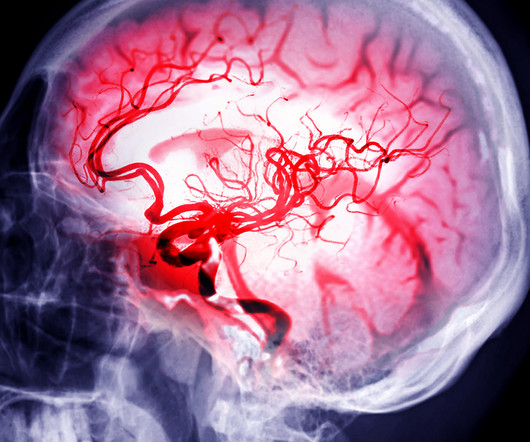
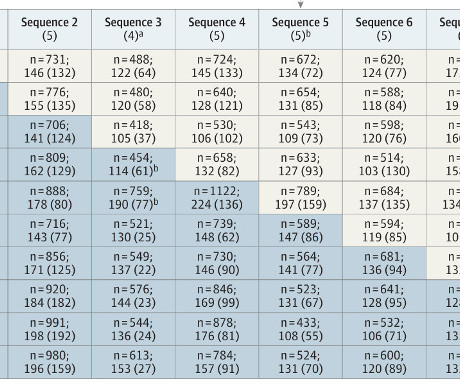
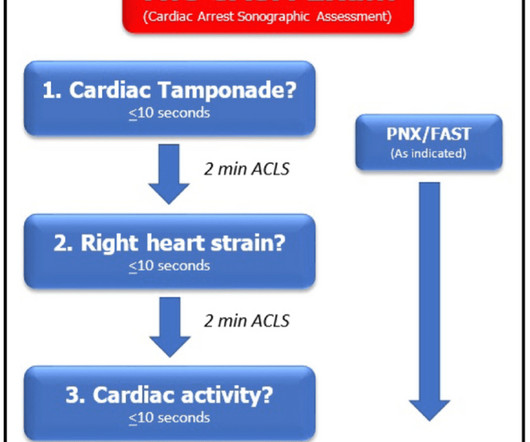
The second part of the analysis involves the downstream outcomes after these patients are seen and/or admitted following their emergency department visit. The authors also tried to evaluate the frequency and outcomes of laboratory and radiology tests ordered by emergency physicians.








































Let's personalize your content