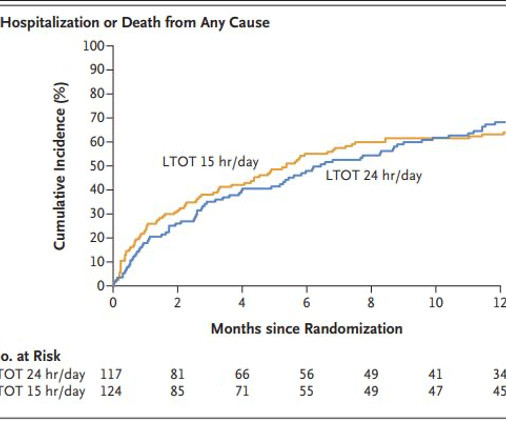
CJEM Visual Abstract – Emergency department crowding negatively influences outcomes for adults presenting with COPD
Canadian EM
MAY 18, 2023
In this issue, we collaborated with CJEM team to present “Emergency department crowding negatively influences outcomes for adults presenting with chronic obstructive pulmonary disease”1 in a visual abstract format. A majority of these patients are affected by chronic obstructive pulmonary disease (COPD).


































Let's personalize your content