Pre-Hospital Antibiotics in Sepsis?
RebelEM
JANUARY 18, 2024
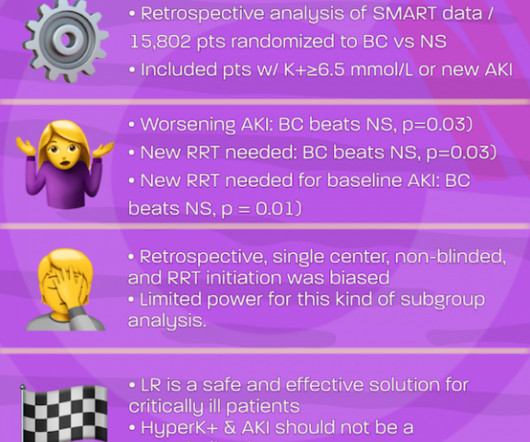
Background: Sepsis remains one of the leading causes of morbidity and mortality. Time to antibiotic therapy (from triage, not from onset of infection) has become a quality metric to improve the time to administration of these medications. Paper: Varney J et al. Health Sci Rep 2022. to 0.97; p = 0.02 to 2.07; p = 0.91 to 0.97; p = 0.02












































Let's personalize your content