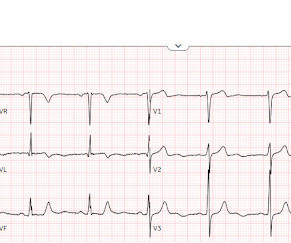
ECG Pointers: STEMI Equivalents from the American College of Cardiology
EMDocs
DECEMBER 11, 2023
As we all know, a critical concern for emergency physicians is identifying patients with heart tissue-threatening ischemia that could benefit from percutaneous catheterization via stent deployment by an interventional cardiologist. The chosen vernacular for these ECG findings has been traditionally called “STEMI equivalents”.


























Let's personalize your content