ECG Blog #366 — Diltiazem didn't work.
Ken Grauer, MD
FEBRUARY 28, 2023
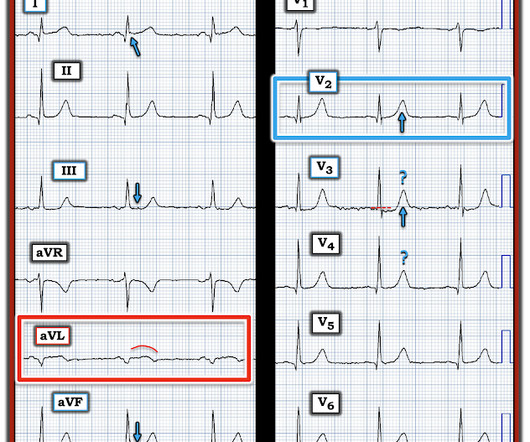
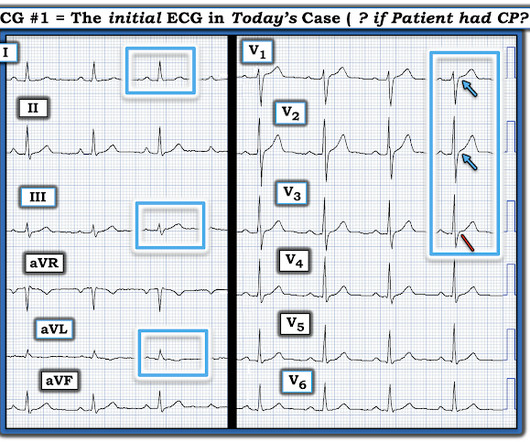
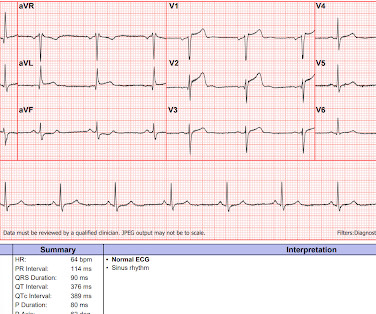
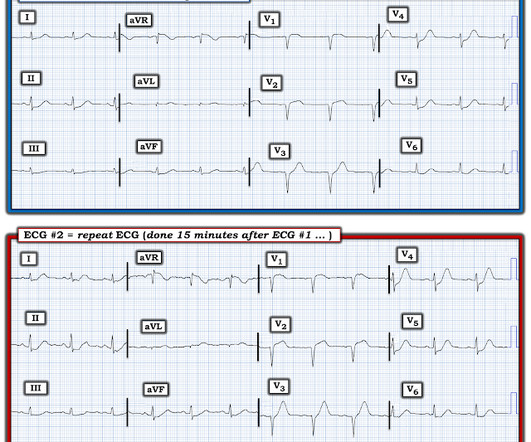
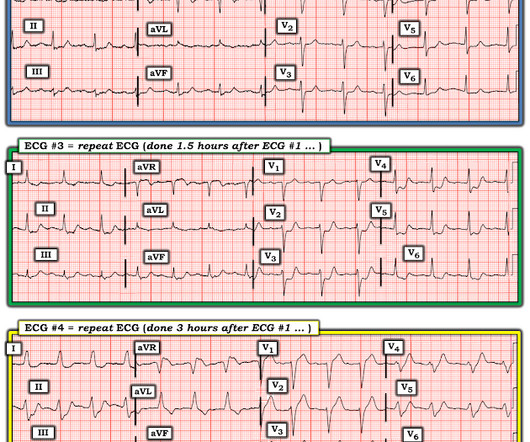
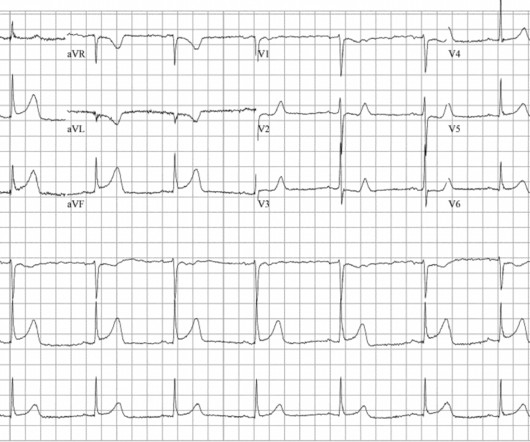
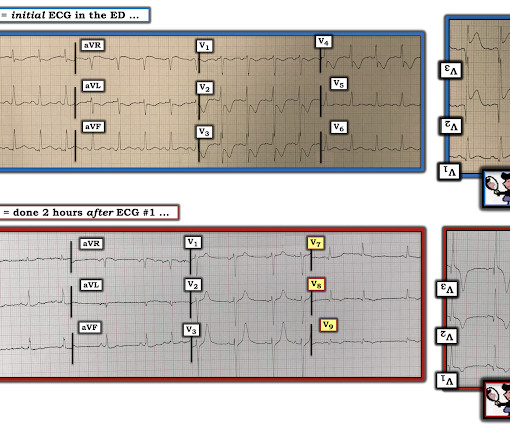
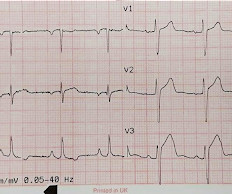
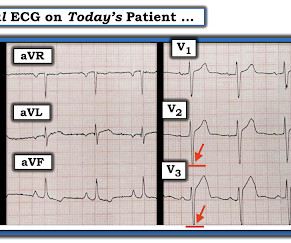
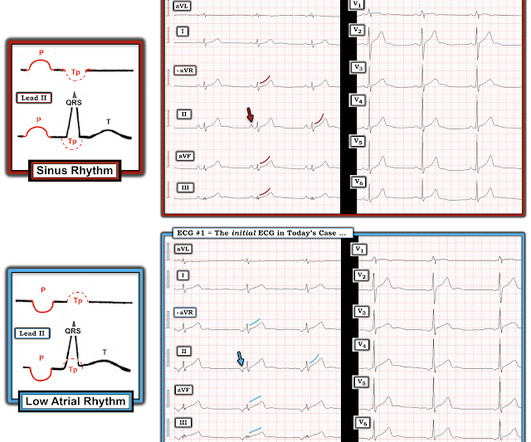
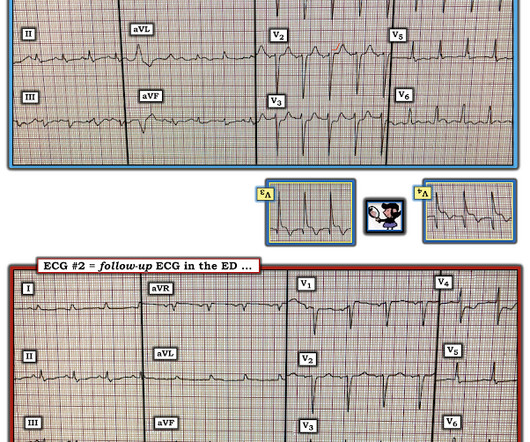
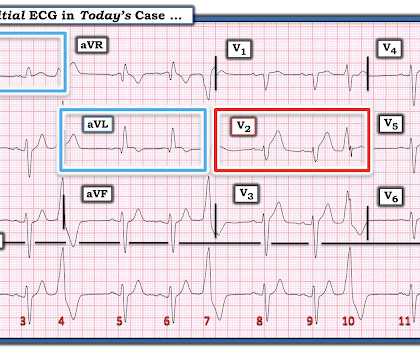
The ECG and long lead II rhythm strip in Figure-1 — was obtained from a COVID positive patient with persistent tachycardia not responding to Diltiazem. Figure-1: The initial ECG — obtained from a patient with persistent tachycardia. ( To improve visualization — I've digitized the original ECG using PMcardio ).




































Let's personalize your content