Ultrasound in Cardiac Arrest
Mount Sinai EM
AUGUST 7, 2024
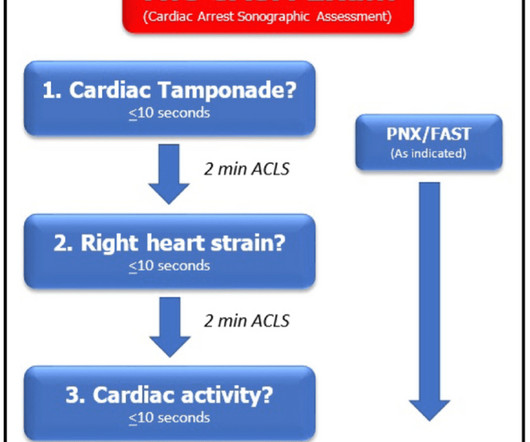
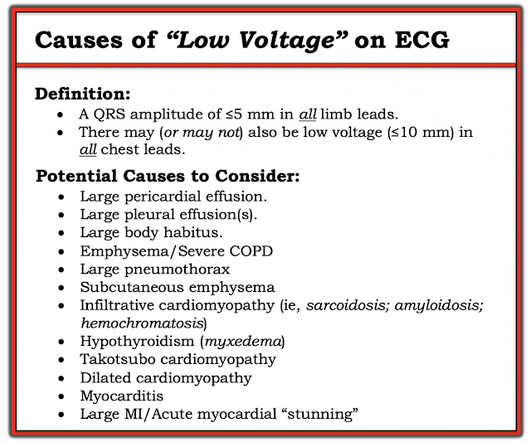
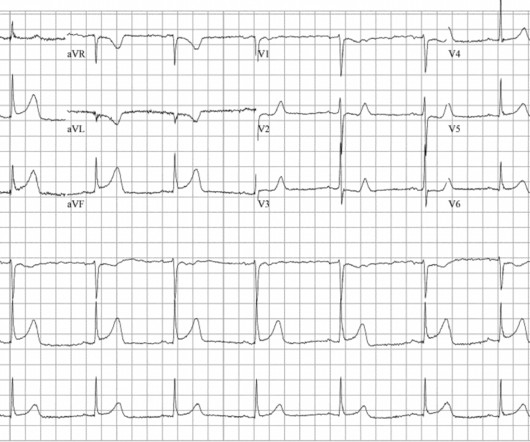
Initially, data suggested that the use of ultrasound during arrest increased pauses between compressions which worsens outcomes. The ideal view depends on the patient’s comorbid conditions such as COPD, obesity, cachexia, etc. Ultrasound during cardiac arrest has quickly become standard.













Let's personalize your content