ECG Blog #432 — "Should I Shock this Patient?"
Ken Grauer, MD
MAY 31, 2024
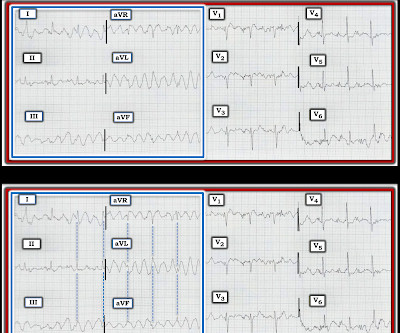
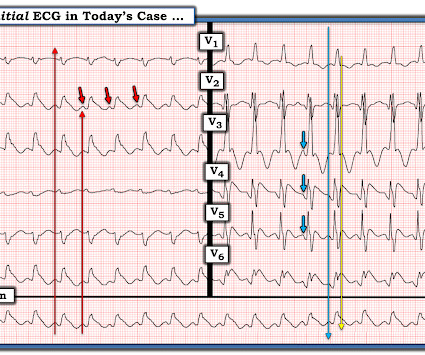
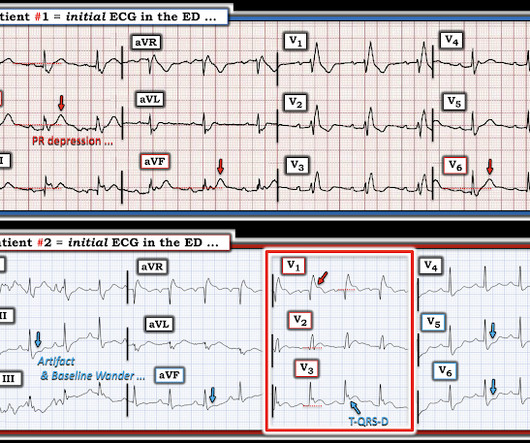
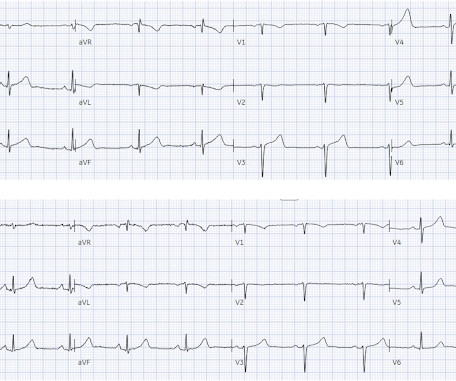
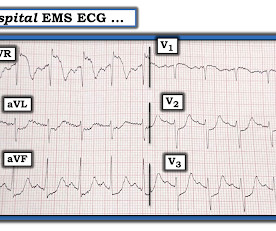
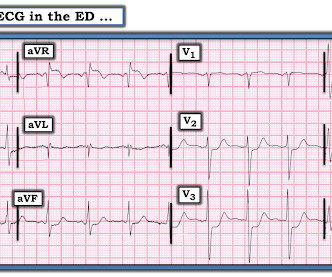
I was sent the ECG in Figure-1 — without the benefit of any history. Figure-1: I was sent this ECG without any history. MY Thoughts on Today’s CASE: As tempting as it might be to reach for the defibrillator on seeing the ECG shown in Figure-1 — My initial reaction was different. No shock was needed. Is this VT?







































Let's personalize your content